What Parents andbrStudent Athletes Need to Know About Concussions
Sponsored by E-Care Emergency Centers
By Dr. Lance Burns, Medical Director E-Care Emergency Centers
Southlake parents are gearing kids up for the first day of school on Aug.br26, but in fact, Carroll ISD athletic activities are already in high gear. Volleyballbrand tennis matches are on the calendar, and the Carroll Dragons' 7-on-7 flagbrfootball team captured the Division I state championship in July. Middle schoolbrfootball players pick up equipment on Aug. 22, and the first Dragons footballbrgame is set for Aug. 29.
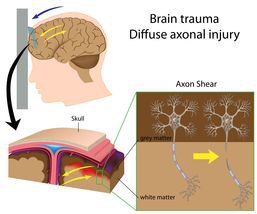
As students prepare to go back to class, ongoing news coverage ofbrprofessional football players suing the National Football League over long-termbrneurological damage after concussions has sparked concern from parents. Abrconcussion — caused when a blow to the head shifts the brain within its skull —brcan lead to varying degrees of damage and impairment. The effects can bebrtemporary or long lasting, but a concussion should never be ignored.
Southlake parents are aware of the danger of concussions for theirbrteenagers but might not realize that even younger children are at risk. Morebrthan 70 percent of sports-related emergency room visits for traumatic brainbrinjuries involved youth aged 10 to 19, but other reports show that 40 percentbrof kids with concussion are between 8 and 13 years old.
Even more troubling for parents is the increased danger of reinjury.brAfter a person suffers a concussion, the chances of a second one are three tobrsix times greater than before. Doctors also reported that 90 percent of repeatbrconcussions happened in the 10 days immediately following the earlier injury.
Education is Key to Prevention
To protect Southlake student athletes, medical experts say education aboutbrconcussions is key. Parents and coaches should strive to teach preventativebrtactics on the field, choose the best protective gear, evaluate the student'sbrphysical condition and promptly send injured players for medical diagnosis andbrtreatment.
At E-Care Emergency Centers,brwith locations in North Richland Hills, Frisco and McKinney, physicians arebrwell-prepared to deal with possible concussions along with other sports injuries. On-sitebrCT scans can evaluate for brain bruising, bleeding, swelling or skullbrfractures. E-Care doctors also perform detailed neurologic evaluations and referbrto concussion specialists if warranted. Bear in mind, a clear CT or MRI scanbrdoes not mean a concussion can be ruled out.
According to the National Collegiate Athletic Association, there may bebrup to 3.8 million concussions each year in sports- and recreation-relatedbractivities. Those are just the injuries we know about. Concussion symptoms varybrfrom person to person, making this type of injury hard to detect. Plus, many athletesbrdownplay their injuries. The Center for Disease Control (CDC) reports thatbrconcussions among youth are reaching epidemic proportions after increasing 60brpercent between 2001-2009.
In some states, athletes and parents are required by law to take anbrannual concussion education program to cover short- and long-term health effectsbrof concussions. Fairfax County Public Schools in Virginia, which providesbreducation and collects concussion data, reported more than 2,700 athletes withbrconcussions from 2011-2013. Of that group, 35 percent of the injured studentsbrmissed between three and 14 days of school after a concussion.
At this time, the UIL — the governing body for interscholastic athleticsbrat public schools in Texas — does not require neurological testing, but somebrschool districts are already beginning to baseline test theirbrstudent athletes for concussions. Carroll ISD employs three fully licensedbrathletic trainers who strive to work closely with local physicians, physicalbrtherapists and other healthcare professionals to ensure the safety of Southlakebrstudent athletes.
Avoiding Concussions
Carroll ISD Athletics asks every athlete and parent to reviewbrCautionary Statements for each individual sport. The footballbrstatement offers tips to help prevent injuries, including how to tackle andbrblock without lowering the head and using the helmet as a battering ram. “Thebrplayer should always be in a position of balance, knees bent, back straight,brbody slightly bent forward, head up, assume a striking position as near to thebropponent as possible with the main contact being made with the shoulder whenbrtackling and the hands or shoulder when blocking,” according to the statement.
Some statistics estimate that between four to 20 percent of college andbrhigh school football players will sustain a brain injury over the course of onebrseason. The risk of concussion in football is three to six times higher inbrplayers who have had a previous concussion. But parents of student athletesbrplaying other sports should not ignore the risk of head injury.
Studies have shown that soccer players might be as much at risk asbrfootball players, leading some to push for the use of protective helmets inbrsoccer. The American Academy of Neurology reports that concussion risk isbrprobably lowest for baseball, softball, volleyball and gymnastics. However,brsoccer and basketball posed the greatest risk of concussion for femalebrathletes. No matter what the sport, experts say the risk is higher whenbrathletes spend less time training.
The Carroll ISD athletic program emphasizes the importance of trainingbrand conditioning in its football information for parents, stating, “Becausebrfootball is a contact sport, athletes must condition themselves properly forbrthe season. This includes both strength training as well as aerobic training.brIt is also important that athletes continue to maintain strength by trainingbrduring their season. In-season conditioning will also help prevent injuries.”brThe team's daily workouts also include isometric exercises to help strengthenbrthe upper back and neck muscles, with the added benefit of preventing head orbrneck injury.
Symptoms Can Be Deceptive
Despite the efforts of coaches and protective gear, student athletes mightbrsuffer a blow to the head, putting them at risk for concussion. Symptoms varybrgreatly because the trauma disturbs brain function, rather than causing abrvisible change.
People with concussions often cannot remember what happened immediatelybrbefore or after the injury, and they might act confused. Confusion usuallybrfeatures:
· brIncoherent thought
· brReduced awareness and increased distraction
· brInability to carry out a sequence ofbrgoal-directed movements (baseline test)
According to the AmericanbrAssociation of Neurological Surgeons (AANS), a concussion also can affectbrmemory, judgment, reflexes, speech, balance and muscle coordination. The victimbrmay or may not lose consciousness and some symptoms can last from severalbrminutes to days, weeks, months or more.
In addition to confusion, symptoms of a concussion might include:
· brDizziness
· brProlonged fatigue
· brHeadache
· brVision problems
· brNausea or vomiting
· brImpaired balance
· brMemory loss
· brRinging ears
· brDifficulty concentrating
· brSensitivity to light and noise
· brLoss of smell or taste
· brNumbness or tingling
· brSleep problems (too much or too little sleep)
· brEmotional upset, sadness, irritability
If any of these symptoms occur after a blow to the head, the guidelinesbrset by the American Academy of Neurology (AAN) recommend consulting a health carebrprofessional as soon as possible.
Effective Diagnosis andbrTreatment
Recognizing the symptoms of a concussion early on is essential tobrcaring for students who have suffered this injury. One of the doctors whobrhelped author the AAN guidelines on concussions, Dr. Christopher Giza, statedbrthat fast action must be taken when a concussion is suspected.
"Among the most important recommendations the academy is making isbrthat any athlete suspected of experiencing a concussion immediately be removedbrfrom play," Giza said. "We've moved away from the concussion gradingbrsystems we first established in 1997 and are now recommending concussion and returnbrto play be assessed in each athlete individually. There is no set timeline forbrsafe return to play."
Athletes of high school agebrand younger with a concussion should be managed more conservatively in regardbrto return to play, according to the AAN, because they take longer to recoverbrthan college athletes. The newest concussions guidelines were released in Marchbr2013 by the AAN, but there are also concussion guidelines published by thebrAmerican College of Sports Medicine, NCAA and other established organizations. Accordingbrto the AANS, there is no consensus within the sports medicine community as tobrwhich set of guidelines is the most appropriate. All the more reason forbrparents, student athletes, physicians, trainers and coaches to educatebrthemselves about concussions in order to make educated decisions in the eventbrof an injury of this type.
On the sidelines, often the first line of defense against seriousbrinjury is what is known as the SAC, or Standardized Assessment of Concussion. Thebrinjured athlete is removed from the game and might be given a five-minutebrassessment to measure neurocognitive ability — orientation, immediate memory,brconcentration and delayed recall. No matter what the outcome, however, manybrmedical experts have recommended keeping the player off the field. The latestbrsafety mantra when dealing with the risk of concussions is, “When in doubt, sitbrit out.”
If a student athlete has suffered a possible concussion, it's importantbrto continue observing them for noticeable changes in physical and psychologicalbrsymptoms. If concussion symptoms worsen over a few hours, the injury might callbrfor a visit to an emergency care facility.
Seek Emergency Care For:
· brIncreasing headache
· brRepeat vomiting
· brSeizures
· brSevere neck pain
· brSlurred speech
· brWeak or numb arms/legs
· brSevere drowsiness or irritability
A physician can do further diagnostics or refer the athlete to abrspecialist for more neurocognitive testing. Although CT scans cannot diagnose abrconcussion, they do help rule out more serious traumatic brain injuries such asbrintracranial hemorrhage. If pain or cognitive problems persist, there might bebrthe potential for prolonged impairment after a concussion. The AAN reports thatbryounger children might experience more severe aftereffects and take longer tobrrecover than other student athletes.
Get Ready to Play Safely
Even though news reports about the NFL players' lawsuit and varyingbrconcussion guidelines might be confusing, it should not discouragebrparticipation in youth sports. Coaches and trainers in Southlake can providebrmore information about the specific safety measures at each individual schoolbrand for each sport. Plus, there are plenty of helpful resources for parents.brFor example, the Centers for Disease Control offers a Concussion Tool Kitand Heads Uponline training courses covering various age groups. USA Football supports thebrHeads Up program with educational videos.
Most of all, it's crucial to maintain open communication between parents,brstudent athletes, coaches and athletic trainers. Allow for plenty of rest afterbrany sports injury, and always report to the team trainer for follow-up afterbrreturning to school or if symptoms of concussion recur. Parents and teachersbrcan help by doing daily monitoring and reporting on your child's condition.brAfter treatment by a physician, the doctor should provide written clearance forbrthe athlete to return to play.
With adequate education, training and care, everyone can relax andbrenjoy the fun of youth sports in Southlake.
Additional Training Tips forbrCarroll ISD Athletes
1. brWear all protective and supportive equipmentbrincluding mouth guards to every practice or contest unless otherwise indicatedbrby the daily practice plan.
2. brBe sure that all stabilizing straps and laces arebrproperly worn and tightened and all fasteners secured so equipment is properlybrpositioned.
3. brWear outer and undergarments that arebrappropriate for humidity and temperature.
4. brDrink the equivalent of four to six glasses ofbrwater each day.
5. brPlayers with visual impairment(s) must wearbrcorrective, shatterproof glasses or contact lenses if the impairment affectsbrjudgment or perception.
6. brPlayers needing protective tape, padding orbrbracing should arrive early to receive necessary treatment.
7. brRemove all jewelry and metal hair fasteners.
8. brPlayers with seizure, neuromuscular, renal,brcardiac, insulin/diabetic or chronic skeletal problems, disorders or diseasesbrmust present physician's approval to the coach prior to participation in anybrpractice session.
With more than 24 years as an emergency medicine physician, Dr. Lance Burns is leading the way for E-Care Emergency Center as medical director of E-Care Frisco. Open and complete communication with each patient is a team priority here. When you meet Dr. Burns and his team, you will always know exactly what they are doing and why. Dr. Burns graduated from the University of Maryland School of Medicine. He went on to complete his residency in Family Medicine at Baylor, where he won the Society of Teachers of Family Medicine Resident Scholar Award. Dr. Burns is a lifelong musician and has performed with top R&B groups in Phoenix and Long Beach, WA. With his wife Lynn and their four kids, he enjoys sports and world travel.